USG-guided Brachial Plexus Block
Unleashing Precision: A Guide to USG-Guided Brachial Plexus Block for Optimal Pain Relief in Regional Anesthesia & Pain Medicine
Introduction
Ultrasound-guided brachial plexus block (US-BPB) has become the gold standard for regional anesthesia in upper limb surgery. While core techniques are well established, ongoing research and innovation continue to refine the approach for improved efficacy, safety, and patient comfort. USG-guided brachial plexus block with 5% Dextrose is also important in chronic pain. This article delves beyond the fundamentals, exploring advanced US-BPB strategies for optimizing outcomes.
What is the Brachial Plexus?
The brachial plexus is a network of nerves in your neck and shoulder that controls feeling and movement throughout your entire arm, from your shoulder to your fingertips. During upper limb surgery, blocking these nerves with local anesthetic ensures a pain-free experience.
Why USG-Guided?
Traditional brachial plexus blocks relied on anatomical landmarks for needle placement. However, these techniques were prone to inaccuracies, potentially leading to incomplete blocks or nerve injury. USG-guided brachial plexus block eliminates this guesswork.
The Power of Ultrasound:
Imagine a real-time map guiding the doctor’s every move. That’s the magic of ultrasound! A high-frequency sound wave creates a detailed image of your anatomy on the screen. The doctor uses this image to visualize the brachial plexus precisely, ensuring the needle targets the exact location for optimal nerve blockade.
Benefits of USG-Guided Brachial Plexus Block:
- Enhanced Accuracy: Ultrasound visualization minimizes the risk of missed blocks or nerve injury.
- Faster Onset: Precise needle placement often leads to a quicker start of pain relief.
- Reduced Complications: USG guidance helps avoid accidental blood vessel puncture.
- Improved Patient Comfort: Knowing exactly where the needle goes reduces anxiety and ensures a more comfortable experience.
Anatomy of the Brachial Plexus
The brachial plexus is organized into five main components: roots, trunks, divisions, cords, and terminal branches. Each component gives rise to specific nerve branches that play crucial roles in innervating the upper extremity.
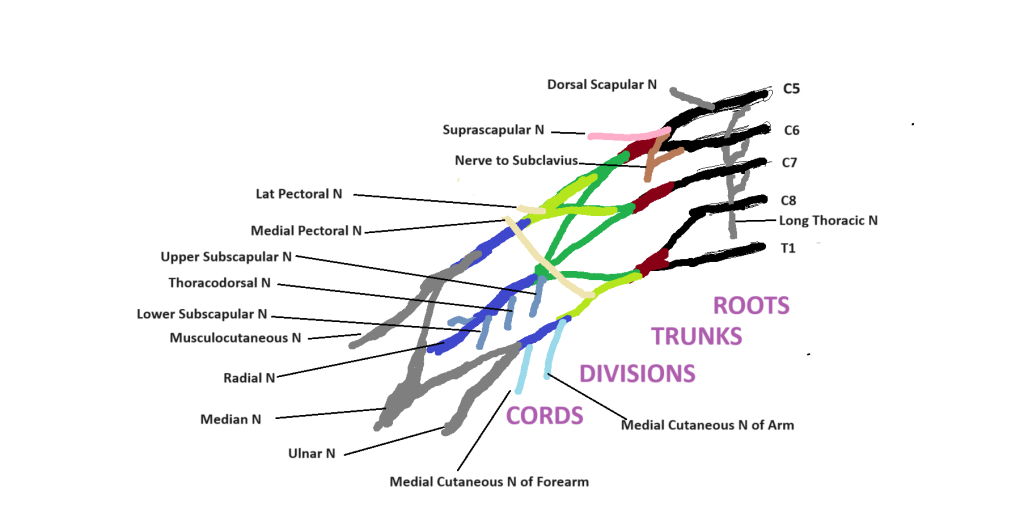
1. Roots
The brachial plexus originates from the anterior rami of spinal nerves C5 to T1. These roots pass between the anterior and middle scalene muscles and give rise to several important branches:
- Dorsal Scapular Nerve (C5): Innervates the rhomboid muscles and the levator scapulae.
- Long Thoracic Nerve (C5, C6, C7): Innervates the serratus anterior muscle.
2. Trunks
The roots converge to form three trunks:
- Upper Trunk: Formed by the union of C5 and C6 roots.
- Branches:
- Suprascapular Nerve: Innervates the supraspinatus and infraspinatus muscles.
- Nerve to Subclavius: Innervates the subclavius muscle.
- Branches:
- Middle Trunk: Continuation of the C7 root.
- Lower Trunk: Formed by the union of C8 and T1 roots.
3. Divisions
Each trunk splits into an anterior and a posterior division:
- Anterior Divisions: Generally supply the flexor muscles of the arm.
- Posterior Divisions: Generally supply the extensor muscles of the arm.
4. Cords
The divisions regroup to form three cords, named according to their relationship to the axillary artery:
- Lateral Cord: Formed by the anterior divisions of the upper and middle trunks.
- Branches:
- Lateral Pectoral Nerve: Innervates the pectoralis major muscle.
- Branches:
- Posterior Cord: Formed by the posterior divisions of all three trunks.
- Branches:
- Upper Subscapular Nerve: Innervates the subscapularis muscle.
- Thoracodorsal Nerve: Innervates the latissimus dorsi muscle.
- Lower Subscapular Nerve: Innervates the subscapularis and teres major muscles.
- Branches:
- Medial Cord: Formed by the anterior division of the lower trunk.
- Branches:
- Medial Pectoral Nerve: Innervates the pectoralis major and minor muscles.
- The Medial Cutaneous Nerve of the Arm: Provides sensory innervation to the skin of the medial arm.
- Medial Cutaneous Nerve of the Forearm: Provides sensory innervation to the skin of the medial forearm.
- Branches:
5. Terminal Branches
The cords give rise to the main terminal branches that innervate the upper limb:
- Musculocutaneous Nerve: Arises from the lateral cord.
- Innervates the coracobrachialis, biceps brachii, and brachialis muscles.
- Continues as the lateral cutaneous nerve of the forearm, providing sensory innervation to the lateral forearm.
- Axillary Nerve: Arises from the posterior cord.
- Innervates the deltoid and teres minor muscles.
- Provides sensory innervation to the skin over the deltoid region (superior lateral cutaneous nerve of the arm).
- Radial Nerve: Arises from the posterior cord.
- Innervates the triceps brachii and the extensor muscles of the forearm.
- Provides sensory innervation to the posterior arm and forearm, and the dorsal surface of the lateral hand.
- Median Nerve: Formed by contributions from both the lateral and medial cords.
- Innervates most of the flexor muscles in the forearm, the thenar muscles, and the lateral two lumbricals.
- Provides sensory innervation to the palmar aspect of the lateral hand and fingers.
- Ulnar Nerve: Arises from the medial cord.
- Innervates the flexor carpi ulnaris, the medial part of the flexor digitorum profundus, and most of the intrinsic hand muscles.
- Provides sensory innervation to the medial part of the hand, including the little finger and the medial half of the ring finger.
Anatomical Landmarks for Ultrasound Guidance
Key anatomical landmarks for ultrasound-guided brachial plexus block include the scalene muscles, subclavian artery, and the first rib. These landmarks help identify the roots and trunks of the brachial plexus. The plexus is typically visualized as a cluster of hypoechoic (dark) oval structures between the scalene muscles.
Techniques of USG-guided Brachial Plexus Block
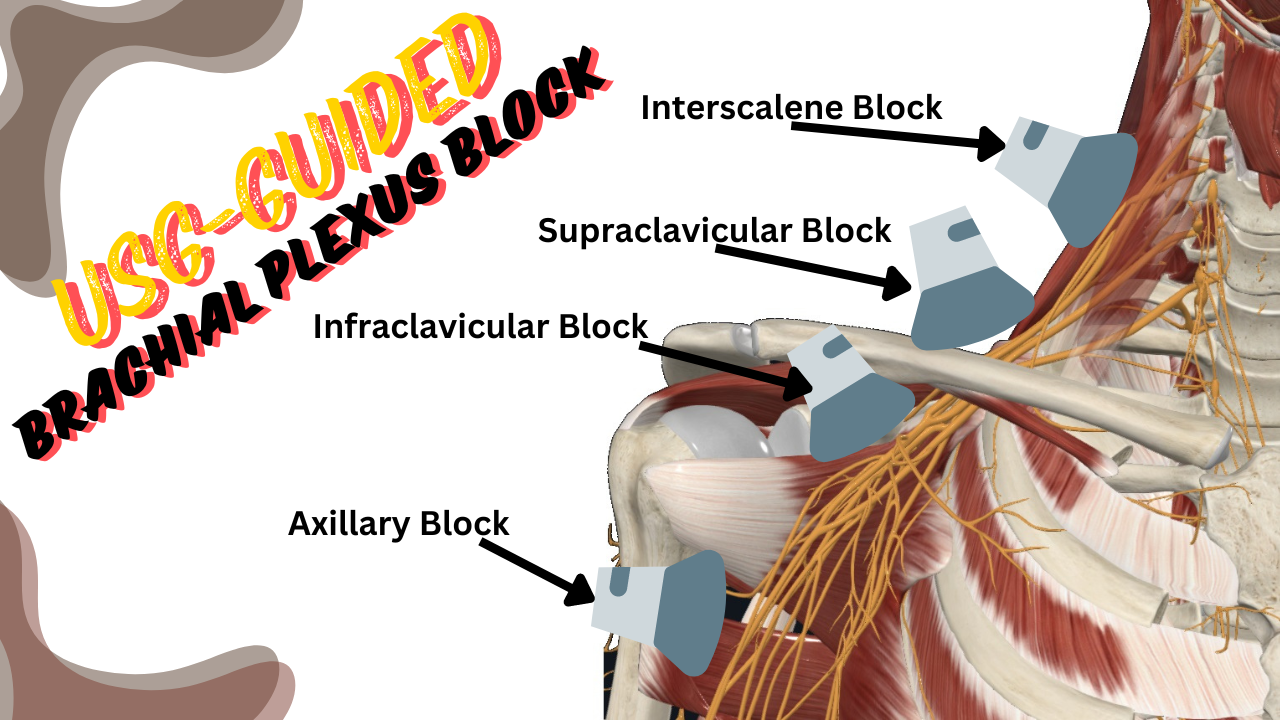
Ultrasound-guided brachial plexus block (USG-guided brachial plexus block) is a widely used regional anesthesia technique for surgeries involving the upper extremities. This technique offers multiple approaches—each targeting different parts of the brachial plexus—providing versatile options for various surgical needs. The four primary approaches include the interscalene, supraclavicular, infraclavicular, and axillary approaches.
- Interscalene Block: Targets the roots/trunks of the brachial plexus at the level of the neck. It is ideal for shoulder and upper arm surgeries.
- Supraclavicular Block: Involves blocking the brachial plexus trunks and divisions at the level of the clavicle. It provides anesthesia for the entire upper limb and is suitable for surgeries of the arm, elbow, and forearm.
- Infraclavicular Block: Targets the cords of the brachial plexus below the clavicle. This approach is beneficial for surgeries of the elbow, forearm, and hand.
- Axillary Block: Blocks the terminal branches of the brachial plexus in the axilla. It is typically used for surgeries of the forearm, wrist, and hand.
1. Interscalene Approach
Anatomical Target
The interscalene approach targets the roots and trunks of the brachial plexus at the level of the C5-C7 nerve roots.
Patient Positioning
- Position: The patient is positioned supine with the head turned slightly away from the side to be blocked.
- Probe Placement: A high-frequency linear ultrasound probe is placed in the transverse plane at the level of the cricoid cartilage, between the anterior and middle scalene muscles.
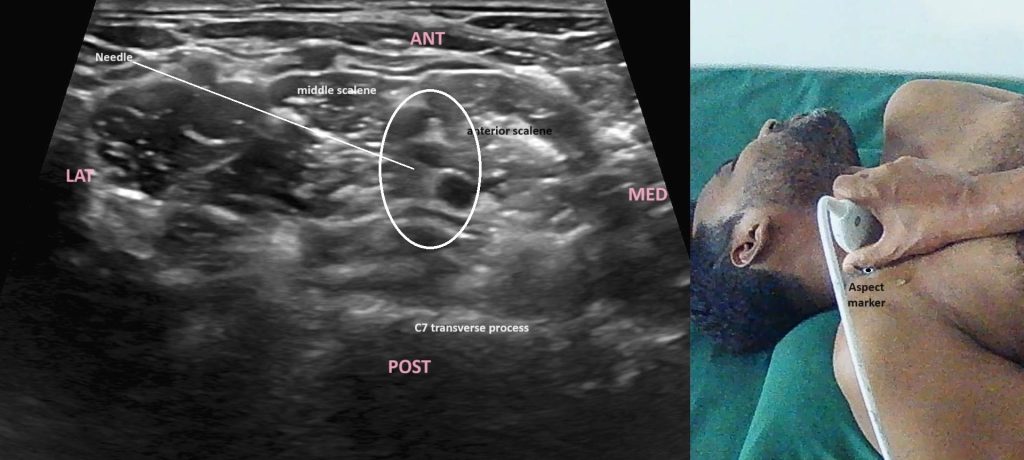
Procedure
- Identification of Structures: Identify the carotid artery, sternocleidomastoid muscle, anterior and middle scalene muscles, and the hypoechoic (dark) nerve roots or trunks between the scalene muscles.
- Needle Insertion: Using an in-plane approach, insert the needle from lateral to medial, directing it towards the interscalene groove where the nerve roots are located.
- Anesthetic Injection: Once the needle tip is adjacent to the nerve roots, inject the local anesthetic while observing its spread around the nerve structures.
Clinical Applications
- Shoulder surgeries
- Upper arm surgeries
- Clavicle surgeries
2. Supraclavicular Approach
Anatomical Target
The supraclavicular approach targets the brachial plexus at the level of the trunks and divisions, just above the clavicle.
Patient Positioning
- Position: The patient is positioned supine with the head turned slightly away from the side to be blocked, and the arm resting comfortably.
- Probe Placement: A high-frequency linear ultrasound probe is placed in the transverse plane above the clavicle, at the midpoint of the clavicle.
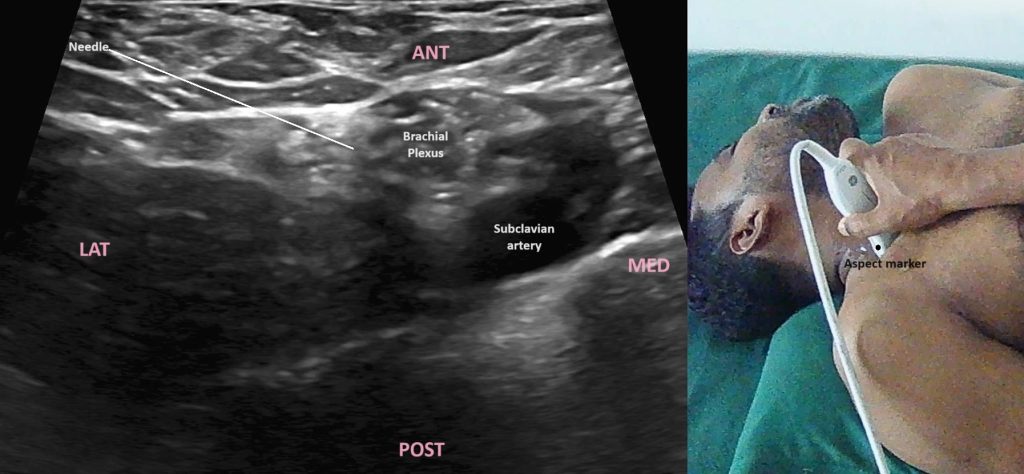
Procedure
- Identification of Structures: Identify the subclavian artery and the brachial plexus, which appears as a cluster of hypoechoic (dark) structures lateral and superior to the artery.
- Needle Insertion: Using an in-plane approach, insert the needle from lateral to medial, directing it towards the cluster of nerves.
- Anesthetic Injection: Once the needle tip is adjacent to the nerve trunks, inject the local anesthetic while observing its spread around the nerve structures.
Clinical Applications
- Upper arm, elbow, and forearm surgeries
- Hand surgeries
3. Infraclavicular Approach
Anatomical Target
The infraclavicular approach targets the brachial plexus at the level of the cords, below the clavicle.
Patient Positioning
- Position: The patient is positioned supine with the arm abducted to 90 degrees and the head turned slightly away from the side to be blocked.
- Probe Placement: A high-frequency linear ultrasound probe is placed in the transverse plane just below the clavicle, lateral to the coracoid process.
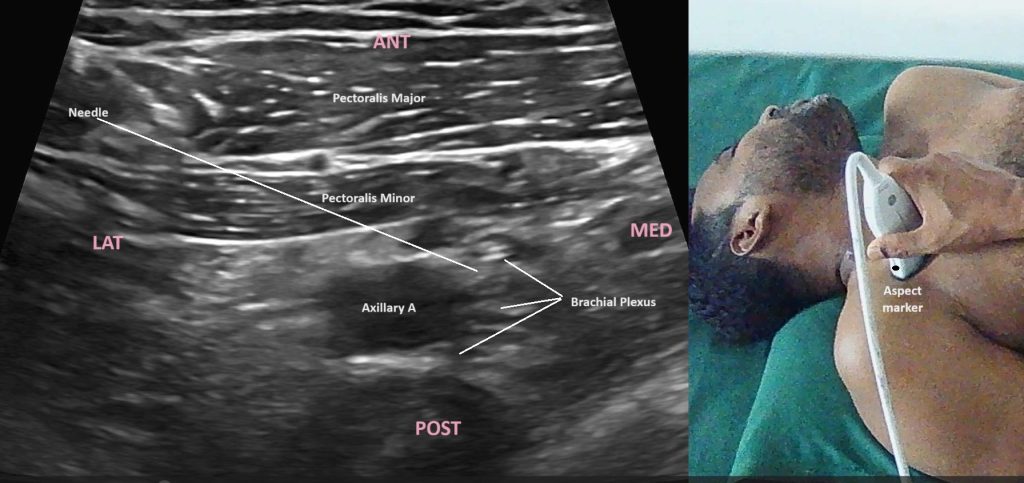
Procedure
- Identification of Structures: Identify the axillary artery and the cords of the brachial plexus, which appear as hypoechoic (dark) structures surrounding the artery.
- Needle Insertion: Using an in-plane approach, insert the needle from superior to inferior, directing it towards the cords.
- Anesthetic Injection: Once the needle tip is adjacent to the cords, inject the local anesthetic while observing its spread around the nerve structures.
Clinical Applications
- Elbow and forearm surgeries
- Hand surgeries
4. Axillary Approach
Anatomical Target
The axillary approach targets the terminal branches of the brachial plexus in the axilla.
Patient Positioning
- Position: The patient is positioned supine with the arm abducted to 90 degrees and the elbow flexed.
- Probe Placement: A high-frequency linear ultrasound probe is placed transversely in the axilla.
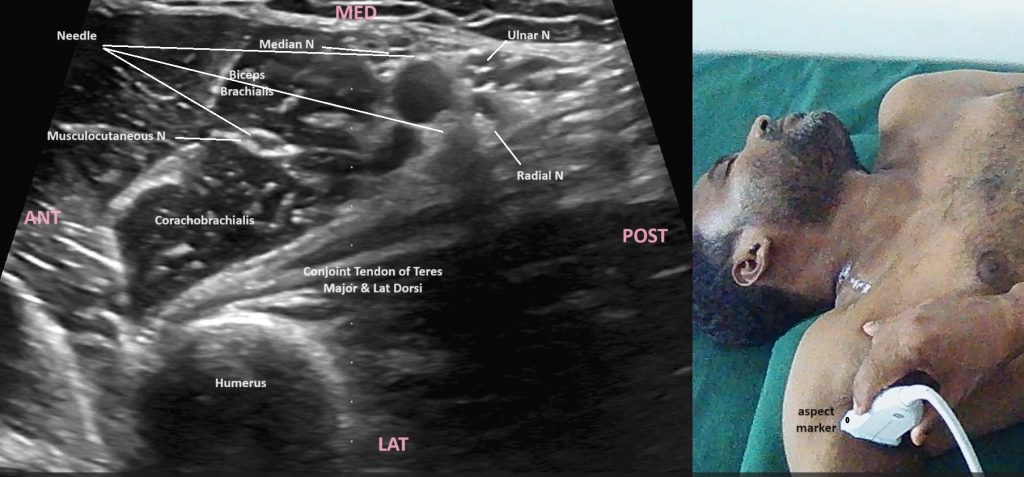
Procedure
- Identification of Structures: Identify the axillary artery and the terminal branches of the brachial plexus, which appear as hypoechoic (dark) structures around the artery.
- Needle Insertion: Using an in-plane approach, insert the needle from lateral to medial, directing it towards the individual nerve branches.
- Anesthetic Injection: Once the needle tip is adjacent to the targeted nerves, inject the local anesthetic while observing its spread around the nerve structures.
Clinical Applications
- Forearm and hand surgeries
Clinical Applications of USG-guided Brachial Plexus Block
USG-guided brachial plexus blocks are used in a variety of clinical settings, including:
- Surgical Anesthesia: Providing anesthesia for surgeries involving the shoulder, arm, forearm, and hand.
- Postoperative Analgesia: Offering prolonged pain relief following upper limb surgeries, thereby reducing the need for systemic opioids.
- Chronic Pain Management: Managing chronic pain conditions such as complex regional pain syndrome (CRPS) and peripheral neuropathies.
- Emergency Settings: Facilitating pain control and allowing for minor surgical procedures in emergency situations.
Benefits of USG-guided brachial plexus block
- Enhanced Accuracy: Direct visualization of the brachial plexus and surrounding structures ensures precise needle placement and local anesthetic administration.
- Reduced Complications: Minimizes the risk of complications such as pneumothorax, vascular puncture, and nerve injury.
- Improved Patient Comfort: Allows for real-time adjustments, reducing the number of needle passes and associated discomfort.
- Better Anesthetic Distribution: Ensures even spread of the anesthetic around the nerves, enhancing the block’s efficacy and duration.
Potential Challenges
Despite its advantages, ultrasound-guided brachial plexus block has some challenges:
- Learning Curve: Requires skill and experience in ultrasound imaging and needle guidance.
- Equipment Dependency: Availability of high-quality ultrasound machines and probes is essential.
- Anatomical Variations: Variations in the anatomy of the brachial plexus can make visualization and needle placement challenging.
- Patient Factors: Obesity, edema, and other patient-specific factors can affect image quality and the ease of performing the block.
Conclusion
Ultrasound-guided brachial plexus block is a transformative technique in regional anesthesia, offering precise, safe, and effective anesthesia and analgesia for upper limb surgeries. Its advantages in terms of accuracy, patient comfort, and reduced complication rates make it a preferred choice among anesthesiologists. While it requires expertise and high-quality equipment, the benefits it provides in enhancing patient outcomes and optimizing pain management are substantial. As technology advances and training improves, ultrasound-guided regional anesthesia is poised to become even more integral to modern anesthetic practice.

