USG-Guided Intercostal Nerve Block
Ultrasound-guided ICN block: Precision Pain Relief for Thoracic Procedures
Introduction
Ultrasound-guided intercostal nerve block (USG-guided intercostal nerve block) is a highly effective technique for managing pain associated with thoracic surgeries, rib fractures, and other chest wall conditions. By utilizing real-time ultrasound imaging, anesthesiologists can accurately target intercostal nerves, providing targeted pain relief with minimal complications. This article explores the detailed aspects of USG-guided intercostal nerve block, including its procedural technique, clinical applications, and benefits.
Anatomy of the Intercostal Nerves
The intercostal nerves play a critical role in providing sensory and motor innervation to the thoracic wall and upper abdominal region. Understanding their anatomy is essential for performing effective regional anesthesia techniques, such as intercostal nerve blocks, used to manage thoracic and upper abdominal pain.
Overview of Intercostal Nerves
Intercostal nerves are the anterior rami of the thoracic spinal nerves T1 to T11. The anterior ramus of the T12 spinal nerve is referred to as the subcostal nerve. These nerves run in the intercostal spaces between the ribs and supply the muscles and skin of the thoracic and abdominal walls.
Origin and Pathway
- Origin: Intercostal nerves originate from the anterior rami of the thoracic spinal nerves.
- Course: After emerging from the intervertebral foramina, the nerves pass between the parietal pleura and the internal intercostal membrane, then run along the inferior margin of each rib.
- Branches: As they progress, intercostal nerves give off several branches, which can be categorized into rami communicantes, collateral branches, lateral cutaneous branches, and anterior cutaneous branches.
Detailed Anatomy
1. Rami Communicantes
Intercostal nerves communicate with the sympathetic trunk via rami communicantes, which consist of:
- White Rami Communicantes: Carry preganglionic sympathetic fibers from the spinal nerve to the sympathetic ganglia.
- Gray Rami Communicantes: Carry postganglionic sympathetic fibers from the sympathetic ganglia back to the spinal nerve.
2. Collateral Branches
- Path: Collateral branches arise near the angle of the rib and descend to run along the superior border of the rib below.
- Function: These branches provide additional innervation to the intercostal muscles and contribute to the sensory supply of the thoracic wall.
3. Lateral Cutaneous Branches
- Path: Lateral cutaneous branches arise near the mid-axillary line, piercing the internal and external intercostal muscles to reach the skin.
- Function: They divide into anterior and posterior branches that supply the skin of the lateral thoracic and abdominal walls.
4. Anterior Cutaneous Branches
- Path: Anterior cutaneous branches arise near the sternum, piercing the internal intercostal muscles and the anterior thoracic wall to reach the skin.
- Function: They divide into medial and lateral branches that supply the skin of the anterior thoracic and abdominal walls.
5. Muscular Branches
- Function: These branches innervate the intercostal muscles (external, internal, and innermost intercostal muscles), the transversus thoracis, the subcostal muscles, and the serratus posterior superior and inferior muscles.
6. Sensory Innervation
- Function: Intercostal nerves provide sensory innervation to the skin overlying the thorax and abdomen, as well as the parietal pleura and the peritoneum.
Specific Thoracic Levels
T1
- Contribution: T1 primarily contributes to the brachial plexus, but a small intercostal branch (first intercostal nerve) supplies the intercostal space.
- Innervation: It provides motor innervation to some intercostal muscles and sensory innervation to the skin of the anterior and lateral chest wall.
T2-T11
- Path: These nerves follow the typical course and branching pattern described above.
- Innervation: They provide motor innervation to the intercostal and abdominal muscles, and sensory innervation to the skin overlying the thorax and abdomen.
T12 (Subcostal Nerve)
- Path: The subcostal nerve follows a similar path but runs below the 12th rib.
- Innervation: It supplies the abdominal muscles and the skin of the lower abdominal wall and upper gluteal region.
Technique of USG-Guided Intercostal Nerve Block
Patient Preparation
- Positioning: The patient is positioned in a sitting or lateral decubitus position to facilitate access to the intercostal spaces.
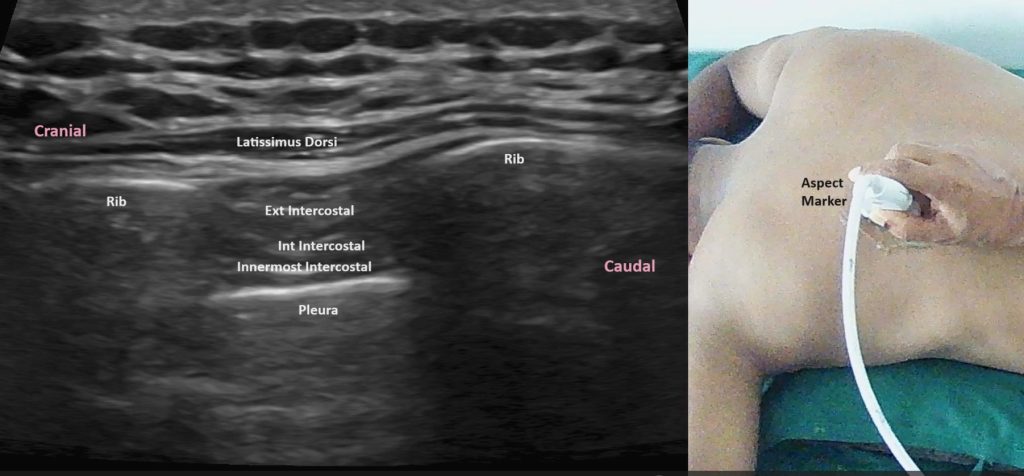
- Equipment: A high-frequency linear ultrasound probe is used to visualize the intercostal spaces and underlying structures.
Procedural Steps
- Probe Placement: Place the ultrasound probe in a longitudinal orientation over the rib in the targeted intercostal space.
- Identification of Structures: Identify the intercostal muscles and ribs. The intercostal nerve, artery, and vein are located in the neurovascular bundle along the inferior border of the rib.
- Needle Insertion: Using an in-plane technique, insert the needle from a caudal to cranial direction, aiming just inferior to the rib. Continuous ultrasound visualization ensures precise needle guidance.
- Confirmation of Needle Placement: The needle tip should be adjacent to the intercostal nerve. Slightly withdraw the needle if bone contact occurs and adjust the needle path to stay in the intercostal space.
- Anesthetic Injection: Slowly inject the local anesthetic, observing its spread within the intercostal space around the nerve. Adequate spread confirms a successful blockade.
Clinical Applications of USG-guided intercostal nerve block
Thoracic Surgery
USG-guided intercostal nerve blocks are invaluable for providing anesthesia and analgesia during thoracic surgeries, including thoracotomies, video-assisted thoracoscopic surgeries (VATS), and breast surgeries. They help reduce postoperative pain and improve patient recovery.
Rib Fractures
Effective pain management is crucial for patients with rib fractures. USG-guided intercostal nerve blocks offer targeted pain relief, facilitating better respiratory function and reducing the risk of complications such as pneumonia.
Chronic Pain Conditions
Intercostal nerve blocks can also manage chronic pain conditions, such as post-thoracotomy pain syndrome, abdominal wall pain and intercostal neuralgia. Ultrasound guidance ensures precise delivery of local anesthetics and steroids, providing long-term pain relief.
Advantages of Ultrasound Guidance
Enhanced Accuracy
Ultrasound guidance allows for direct visualization of the intercostal nerves and surrounding structures, ensuring precise needle placement. This reduces the risk of complications, such as pneumothorax and vascular puncture.
Improved Patient Safety
Real-time imaging minimizes the likelihood of inadvertent injury to adjacent structures, enhancing overall patient safety. The ability to observe the spread of the anesthetic further confirms the success of the block.
Superior Analgesia
The precise delivery of local anesthetic ensures optimal nerve blockade, resulting in superior pain control. This is particularly beneficial for postoperative pain management and chronic pain conditions.
Reduced Opioid Consumption
Effective regional anesthesia with USG-guided intercostal nerve blocks reduces the need for systemic opioids, minimizing the risk of opioid-related side effects, dependency, and overdose. This approach aligns with current efforts to address the opioid epidemic.
Potential Challenges of USG-guided Intercostal Nerve Block
Learning Curve
Proficiency in ultrasound-guided techniques requires dedicated training and practice. Anesthesiologists must develop skills in ultrasound imaging, needle guidance, and interpretation of sonographic anatomy. Simulation training and hands-on workshops can help overcome this learning curve.
Equipment Availability
High-quality ultrasound machines and appropriate probes are essential for successful ultrasound-guided intercostal nerve blocks. Access to such equipment may vary between institutions, potentially limiting the widespread adoption of these techniques.
Anatomical Variations
Variations in intercostal nerve anatomy can pose challenges to successful blockade. Anesthesiologists must be adept at identifying and adapting to these variations to ensure effective anesthesia.
Conclusion
Ultrasound-guided intercostal nerve block (USG-guided intercostal nerve block) represents a significant advancement in regional anesthesia and pain management for thoracic conditions. Its ability to provide precise, safe, and effective pain relief makes it an invaluable tool in clinical practice. By reducing reliance on systemic opioids and improving patient outcomes, this technique enhances the quality of care for patients undergoing thoracic procedures or suffering from chronic thoracic pain. Despite challenges such as the learning curve and equipment requirements, the benefits of USG-guided intercostal nerve blocks far outweigh these obstacles, solidifying their role in modern anesthetic practice.

