USG-Guided Tibial Nerve Block
Ultrasound-Guided Tibial Nerve Block at Ankle in Regional Anesthesia and Pain Medicine
Introduction
Unveiling the Tibial Nerve:
The tibial nerve, a branch of the sciatic nerve, courses posteriorly through the leg, innervating the plantar aspect of the foot and the majority of the toes. Precise blockade of this nerve is crucial for achieving profound anesthesia during various foot and ankle surgeries, and pain interventions.
The Power of Ultrasound Guidance:
USG-guided tibial nerve block transcends the limitations of traditional techniques. By utilizing a high-frequency sound wave, a real-time image of the ankle anatomy is displayed on the screen. This meticulous visualization empowers you to:
- Identify the Tibial Nerve with Unequivocal Precision: Visualize the tibial nerve in its entirety, eliminating the guesswork associated with anatomical landmarks.
- Navigate Bony Prominence with Confidence: The ultrasound image clearly depicts the posterior tibial artery and the flexor retinaculum, guiding safe needle placement around these structures.
- Target Specific Branches (Optional): In certain procedures, the medial and lateral plantar nerves, branches of the tibial nerve, can be selectively targeted for even more refined anesthesia.
- Minimize Risk of Complications: Ultrasound guidance significantly reduces the potential for inadvertent vascular puncture or intraneural injection.
Optimizing Your USG-Guided Tibial Nerve Block Technique:
- Needle Selection: A high-frequency linear ultrasound probe (10-15 MHz) is used for optimal visualization. A 22-gauge or 25-gauge short bevel needle is preferred for the block.
- Patient Positioning: The patient can be positioned either prone or supine with the foot in dorsiflexion.exclamation
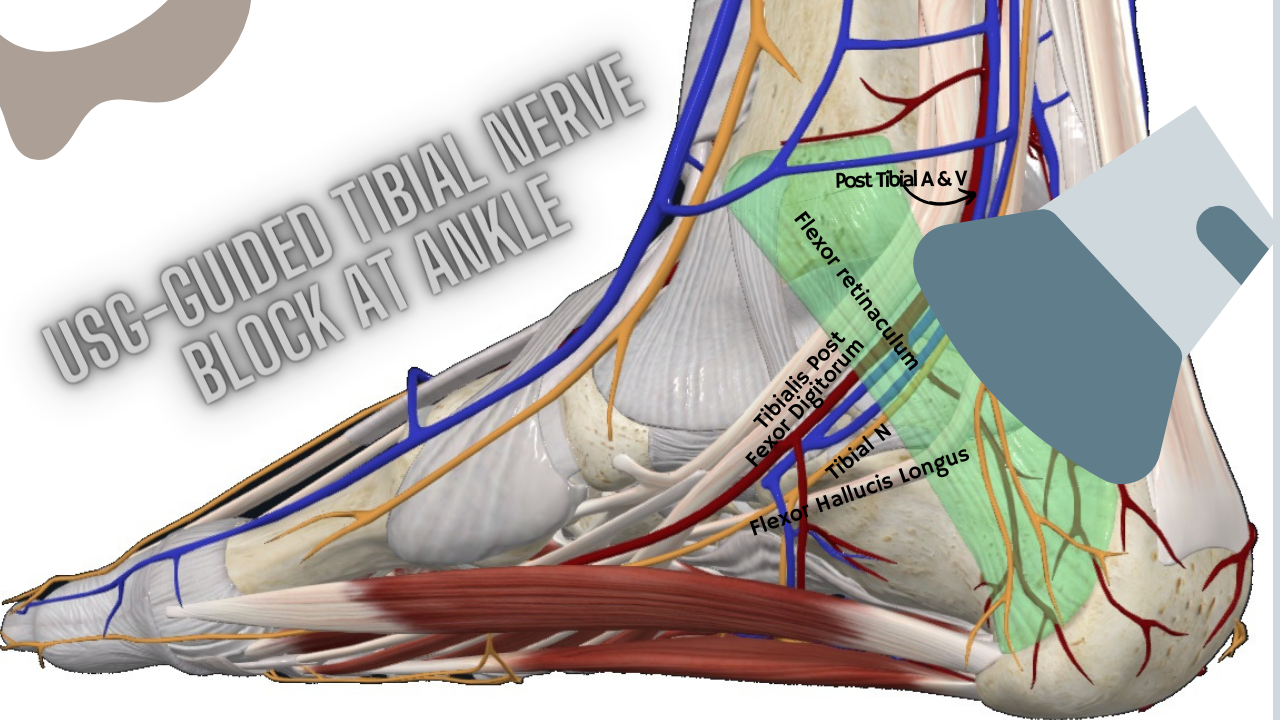
- Ultrasound Imaging: Locate the tibial nerve posterior to the medial malleolus, deep to the flexor retinaculum, and nestled between the tendons of the tibialis posterior and flexor digitorum longus muscles.
- Needle Insertion: Using an in-plane technique, insert the needle under direct ultrasound visualization, ensuring the entire needle trajectory is visualized.
- Local Anesthetic Injection: Once the needle tip is adjacent to the tibial nerve, inject a small test dose of local anesthetic with epinephrine.exclamation A negative aspiration test helps confirm extravascular placement. Subsequently, inject the desired volume of local anesthetic solution (typically 3-5 mL).exclamation
Advanced Techniques for Enhanced Outcomes:
- Hydrodynamic Dissection (HD): This technique utilizes a high volume of local anesthetic solution with a blunt needle tip to create a space around the nerve, facilitating even distribution of the anesthetic and potentially leading to a faster onset of action.
- Continuous Tibial Nerve Block: For extended pain management post-operatively, consider placement of a continuous peripheral nerve catheter under ultrasound guidance. This allows for continuous local anesthetic infusion for prolonged analgesia.
Detailed Anatomy of the Tibial Nerve
Origin and Course
- Roots: The tibial nerve originates from the L4 to S3 spinal nerve roots.
- Sciatic Nerve: It is a branch of the sciatic nerve, which bifurcates into the tibial and common peroneal nerves.
- Popliteal Fossa: The tibial nerve descends through the popliteal fossa.
- Posterior Leg: It continues down the posterior compartment of the leg.
- Medial Malleolus: The nerve passes posterior to the medial malleolus at the ankle.
Anatomical Landmarks at the Ankle
- Medial Malleolus: The bony prominence on the inner aspect of the ankle.
- Flexor Retinaculum: A fibrous band that covers the tarsal tunnel.
- Tarsal Tunnel: A passageway formed by the flexor retinaculum where the tibial nerve, posterior tibial artery, and veins pass into the foot.
- Posterior Tibial Artery: Runs alongside the tibial nerve and serves as a useful landmark during ultrasound-guided procedures.
Branches
- Medial Plantar Nerve: Supplies the medial aspect of the sole and the first three and a half toes.
- Lateral Plantar Nerve: Supplies the lateral aspect of the sole and the last one and a half toes.
- Calcaneal Branches: Innervate the skin of the heel.
Ultrasound-Guided Tibial Nerve Block (USG-Guided Tibial Nerve Block)
Indications of USG-Guided Tibial Nerve Block
- Surgical Procedures: Used for surgeries involving the foot and ankle, such as bunionectomy, toe amputations, and Achilles tendon repair.
- Postoperative Pain Management: Provides effective analgesia following foot and ankle surgeries.
- Chronic Pain Conditions: Particularly useful for managing tarsal tunnel syndrome, plantar fasciitis, and neuropathic pain.
Technique of USG-Guided Tibial Nerve Block

- Patient Positioning: The patient is positioned supine with the leg slightly externally rotated to expose the medial aspect of the ankle.
- Equipment:
- High-frequency linear ultrasound transducer (10-15 MHz).
- 22-25 gauge, 50 mm nerve block needle.
- Local anesthetic (e.g., lidocaine for short duration, bupivacaine for longer duration).
- Preparation:
- Clean the skin with antiseptic solution.
- Apply a sterile ultrasound gel and place the transducer transversely just proximal to the medial malleolus.
- Ultrasound Identification:
- Identify the posterior tibial artery, which appears as an anechoic (dark) pulsating structure.
- Locate the tibial nerve as a round, hyperechoic (bright) structure just posterior to the artery.
- Needle Insertion:
- Insert the needle in-plane with the ultrasound transducer, advancing it towards the tibial nerve.
- Ensure the needle tip is adjacent to the nerve without piercing it.
- Injection:
- Aspirate to ensure the needle is not in a blood vessel.
- Inject 5-10 mL of local anesthetic around the nerve, observing the spread of the anesthetic under ultrasound.
Confirmation of Block
- Sensory Testing: Loss of sensation in the sole of the foot and the plantar aspect of the toes.
- Motor Testing: Weakness or inability to plantar flex the foot.
Tarsal Tunnel Syndrome and USG-Guided Tibial Nerve Block
Overview of Tarsal Tunnel Syndrome
- Definition: A compressive neuropathy of the tibial nerve as it passes through the tarsal tunnel.
- Symptoms: Pain, tingling, and numbness in the sole of the foot, often exacerbated by activity and relieved by rest.
Pathophysiology
- Compression: The tibial nerve can be compressed by structures within the tarsal tunnel, such as swollen tendons, cysts, or varicose veins.
- Inflammation: Inflammatory conditions such as rheumatoid arthritis can contribute to nerve compression.
Diagnosis
- Clinical Examination: Symptoms are often reproduced by tapping over the tarsal tunnel (Tinel’s sign).
- Imaging: Ultrasound and MRI can help identify compressive structures.
Role of USG-Guided Tibial Nerve Block
- Diagnostic Block: A tibial nerve block can help confirm the diagnosis by temporarily relieving symptoms.
- Therapeutic Block: Provides pain relief and can reduce inflammation, aiding in the treatment of tarsal tunnel syndrome.
Advantages of Ultrasound Guidance
- Increased Accuracy: Direct visualization of the nerve and surrounding structures ensures precise placement of the needle.
- Enhanced Safety: Reduces the risk of inadvertent vascular puncture and nerve injury.
- Effective Analgesia: Provides superior pain relief compared to blind or landmark-based techniques.
Potential Complications
- Infection: Maintaining a sterile technique reduces the risk.
- Hematoma: Careful needle placement and aspiration minimize the risk.
- Nerve Injury: Avoiding direct needle contact with the nerve mitigates this risk.
- Local Anesthetic Toxicity: Using appropriate doses and incremental injection techniques helps prevent systemic toxicity.
Conclusion
The USG-guided tibial nerve block at the ankle is a highly effective and safe technique for providing regional anesthesia and managing pain, particularly in conditions like tarsal tunnel syndrome. Mastering the detailed anatomy of the tibial nerve and the ultrasound-guided technique is essential for ensuring successful blocks and optimal patient outcomes. By leveraging the advantages of ultrasound guidance, clinicians can significantly enhance the efficacy and safety of tibial nerve blocks, providing superior pain relief and improving the overall quality of care.

